Understanding SOAP Notes in Nursing

In the world of nursing, accurate and comprehensive documentation is paramount to ensuring quality patient care. Among the various methods used for recording patient information, SOAP notes hold a prominent place. SOAP notes provide a standardized format, following a defined structure that encompasses subjective, objective, assessment, and plan sections. This format facilitates effective communication among healthcare professionals, ensuring seamless collaboration and continuity of care. In this comprehensive guide, we will delve into the purpose and structure of SOAP notes in nursing, while incorporating practical examples related to anxiety and depression. By examining sample SOAP notes for anxiety and depression, we will demonstrate how this documentation method can be applied in real-life scenarios. Additionally, we will discuss the significance of SOAP notes in psychotherapy, where they serve as valuable tools for tracking progress and tailoring treatment plans to individual needs. Join us as we embark on a journey through the realm of SOAP notes in nursing and counseling, where meticulous documentation paves the way for exceptional patient outcomes.
The significance of SOAP notes cannot be overstated when it comes to nursing documentation. These notes serve as a vital communication tool, fostering effective collaboration and information exchange among healthcare professionals. By adhering to a standardized format, which includes subjective, objective, assessment, and plan sections, SOAP notes ensure consistency and clarity in documenting patient information, allowing for easy interpretation and seamless transitions in care. Whether documenting an anxiety soap note, a depression soap note, or any other mental health-related condition, SOAP notes provide a structured framework for capturing the patient’s subjective experiences and objective data. They enable thorough assessments by incorporating relevant details and observations, such as symptoms, behaviors, and vital signs. Through SOAP notes, nurses can document their assessments for soap note documentation while capturing important factors specific to anxiety, depression, and other conditions. In our exploration of SOAP notes in this guide, we will specifically examine how they can assist in assessing and managing anxiety and depression, two prevalent mental health conditions that require diligent monitoring and intervention. Additionally, we will shed light on the role of SOAP notes in the context of psychotherapy, where they serve as a valuable tool for tracking therapeutic progress and tailoring treatment plans to meet individual needs. By utilizing SOAP notes in counseling sessions, therapists can document the effectiveness of interventions, track changes over time, and collaborate effectively with other healthcare professionals. Get ready to unravel the intricacies of SOAP notes in nursing as we equip you with the knowledge and tools to optimize your documentation practices and enhance patient-centered care.
The Significance of SOAP Notes in Nursing
In the dynamic field of nursing, accurate and comprehensive documentation is crucial for providing quality patient care. Among the various methods used for recording patient information, SOAP notes hold a prominent place. SOAP notes play a critical role in nursing practice by documenting patients’ subjective and objective data, assessments, and plans in a structured and standardized format. These notes ensure continuity of care and effective communication among nurses, physicians, and other healthcare providers. Moreover, SOAP notes serve as a valuable resource for assessing anxiety and depression, allowing nurses to address mental health concerns comprehensively. By incorporating key details related to these conditions, such as an anxiety soap note example or a sample soap note for anxiety, nurses can seamlessly integrate their assessment for soap note documentation and provide holistic care to patients in need. Join us in this comprehensive guide as we explore the purpose, structure, and significance of SOAP notes in nursing, shedding light on their invaluable role in assessing and managing anxiety and depression through psychotherapy soap notes.
SOAP notes ensure continuity of care and effective communication by providing a standardized framework for documenting patients’ subjective and objective data, assessments, and plans. These notes serve as a comprehensive resource for healthcare providers, particularly when it comes to assessing and addressing mental health concerns such as anxiety and depression. Within the SOAP note format, nurses can capture vital information related to the patient’s subjective experiences, symptoms, and concerns associated with anxiety and depression. By incorporating soap note anxiety and soap note counseling, nurses can accurately document and monitor the progress of patients’ mental well-being. Moreover, utilizing soap note examples for depression or soap notes therapy examples, nurses can develop well-informed assessments and tailored plans to address mental health issues comprehensively. The structured nature of SOAP notes, along with soap note format and soap notes meaning, ensures that essential information is recorded, facilitating effective communication among healthcare professionals and enhancing the quality of patient care. As we explore the realm of SOAP notes in nursing, we will highlight their significance in assessing and managing anxiety and depression through psychotherapy soap notes, empowering nurses to provide holistic care and support to individuals in need.
The Structure of SOAP Notes
SOAP notes follow a structured format that includes subjective, objective, assessment, and plan sections, playing a vital role in medical documentation. In the realm of nursing, SOAP notes serve as a comprehensive tool for capturing patient information and facilitating effective communication among healthcare professionals. Let’s explore how each section can be incorporated into nursing practice while considering anxiety and depression scenarios. When documenting an anxiety soap note or a depression soap note, nurses can utilize soap note examples for anxiety and depression to guide their documentation process.
The subjective section allows nurses to capture the patient’s self-reported experiences, thoughts, and concerns related to anxiety and depression, providing valuable insights into their mental health. By incorporating assessment for soap note documentation, nurses can systematically evaluate the patient’s symptoms, behaviors, and responses to treatment. In the objective section, nurses document objective data, such as vital signs, physical examinations, and laboratory results, providing a comprehensive picture of the patient’s condition. With soap note counseling and soap therapy notes, nurses can outline counseling interventions, therapy modalities, and progress in the plan section, tailoring treatment plans to address anxiety and depression effectively. SOAP notes in counseling and therapy enable therapists to document the progress, challenges, and achievements of their clients. By adhering to the soap note format and utilizing soap notes examples, nurses and therapists can ensure consistency, accuracy, and meaningful documentation. The significance of SOAP notes in counseling lies in their ability to provide a comprehensive overview of the client’s mental health journey, facilitating collaboration with other healthcare providers. Hence, SOAP notes in nursing and counseling serve as invaluable tools for documenting, assessing, and managing anxiety and depression, enabling personalized care and supporting positive patient outcomes.
Subjective

In the subjective section of a SOAP note, nurses diligently document patients’ self-reported symptoms and concerns, utilizing a standardized format known as SOAP notes. This documentation method is essential for effective communication and comprehensive patient care. When assessing anxiety, nurses can draw inspiration from an anxiety soap note example to structure their notes appropriately. By incorporating key details into the subjective section, such as persistent worry, restlessness, and difficulty concentrating, nurses ensure a thorough assessment. Similarly, in addressing depression, nurses can refer to a depression soap note example to guide their documentation process.
Including information such as feelings of profound sadness, loss of interest in activities, and changes in appetite allows for a comprehensive evaluation of the patient’s emotional well-being. By adhering to the soap note format, nurses ensure standardized documentation that aids in assessment and treatment planning. These SOAP notes in nursing, counseling, and psychotherapy serve as a vital tool for capturing and communicating patient information effectively. Whether it is utilizing soap notes counseling for therapeutic interventions or using soap notes therapy examples as a reference, nurses can provide comprehensive care by integrating the appropriate SOAP note elements. Understanding the meaning and significance of SOAP notes in counseling and therapy is paramount, as these notes facilitate continuity of care and enhance collaboration among healthcare providers. By utilizing soap notes templates and following soap documentation guidelines, nurses can document subjective information in a standardized manner, ultimately improving patient outcomes and ensuring the provision of high-quality care.
Objective
In the objective section of a SOAP note, nurses demonstrate their proficiency in incorporating various components, including anxiety and depression, to provide a comprehensive assessment. By referencing an anxiety soap note example, nurses can effectively structure their objective observations. Measurable data such as vital signs, physical manifestations, and behavioral observations form the foundation of this section. For instance, when assessing anxiety, nurses can document specific findings like an increased heart rate (120 bpm), trembling hands, and hyperventilation. These objective indicators help establish the severity and physiological impact of anxiety, supporting accurate assessment and treatment planning. Similarly, when addressing depression, nurses can draw inspiration from a depression soap note example to capture observable behaviors associated with this condition.
Objective observations may include a slumped posture, slowed motor movements, and tearfulness during interactions. By incorporating these detailed observations into the objective section, nurses provide valuable insight into the emotional and physical manifestations of depression. SOAP notes, a standardized documentation method in healthcare, ensure that nurses adhere to a consistent format, promoting clarity and effective communication. By following soap documentation guidelines and utilizing soap notes templates, nurses demonstrate their proficiency in documenting objective data related to anxiety and depression. These SOAP notes serve as essential tools for healthcare professionals, allowing for a comprehensive evaluation of patients’ mental health conditions. With their holistic approach and significance in counseling and therapy, SOAP notes play a pivotal role in providing quality care and facilitating collaboration among healthcare providers.
Assessment
In the assessment section of a SOAP note, nurses demonstrate their expertise in utilizing SOAP documentation to provide a comprehensive evaluation of the patient’s condition. Incorporating elements from anxiety soap notes and depression soap notes, nurses ensure accurate assessments and promote effective treatment planning. When addressing anxiety, nurses integrate the patient’s self-report and observed symptoms, adhering to the SOAP note format. For instance, a well-rounded assessment statement may include the following: “Based on the patient’s self-report of persistent worry, restlessness, and difficulty concentrating (subjective), along with observed symptoms of increased heart rate, trembling hands, and hyperventilation (objective), anxiety disorder is suspected. Further assessment and collaboration with a mental health professional are recommended to confirm the diagnosis and develop an appropriate treatment plan.”
By utilizing SOAP notes in counseling and therapy, nurses provide a comprehensive evaluation that incorporates both subjective and objective information. Similarly, when evaluating depression, nurses apply their knowledge and expertise to assess the patient’s symptoms accurately. By following the SOAP note format, an assessment statement could be: “The patient’s self-report of profound sadness, loss of interest in previously enjoyed activities, along with observed symptoms of a slumped posture, slowed motor movements, and tearfulness, indicate that the patient’s symptoms meet the criteria for major depressive disorder. Referral to a psychiatrist for evaluation and possible medication management is advised to support the patient’s recovery and improve their overall quality of life.” By seamlessly incorporating the keywords and concepts related to SOAP notes in counseling and medical practice, nurses ensure that their assessments are thorough, informative, and conducive to collaborative care.
Plan

In the realm of nursing and counseling, anxiety soap notes and depression soap notes serve as vital tools for effective documentation and comprehensive patient care. These SOAP notes, adhering to a structured format, provide a standardized method of documenting subjective and objective information, assessments, and plans. By incorporating the principles of soap documentation and utilizing soap method charting, healthcare professionals ensure accurate and consistent recording of patient data.
An anxiety soap note example may involve documenting the patient’s self-reported symptoms and concerns related to anxiety, along with objective observations and assessments. For instance, the nurse may record the patient’s reports of persistent worry, restlessness, and difficulty concentrating in the subjective section of the note. In the objective section, vital signs and physical manifestations such as increased heart rate, trembling hands, and hyperventilation could be documented.
Similarly, in a depression soap note example, nurses capture the patient’s self-reported feelings and observable signs of depression. The subjective section may include statements such as the patient expressing sadness, loss of interest in activities, and changes in appetite. In the objective section, nurses may note physical observations like slumped posture, slowed motor movements, and tearfulness.
The SOAP note format, particularly in counseling, holds significance in psychotherapy and allows for the integration of therapy-focused interventions. The plan section of the soap note for anxiety may include actions such as psychoeducation on stress management techniques, referral to a therapist for cognitive-behavioral therapy, and monitoring medication adherence if prescribed. For depression, the plan may involve implementing daily mood assessments, encouraging engagement in pleasurable activities, coordinating support groups, and collaborating with the care team for potential medication adjustment.
By following the soap notes counseling template, nurses create a comprehensive and individualized approach to patient care. These soap notes therapy examples support continuity of care, facilitate effective communication among healthcare professionals, and ensure the holistic management of anxiety and depression. With an understanding of what soap notes are in counseling and their meaning, nurses can confidently utilize this documentation method to address the diverse needs of patients and foster their well-being.
Conclusion
In conclusion, embracing the use of SOAP notes in nursing is crucial for delivering exceptional patient care. By incorporating these standardized and structured documentation practices, healthcare professionals can effectively communicate, track progress, and tailor treatment plans for individuals with anxiety and depression. SOAP notes provide a comprehensive framework for recording subjective and objective data, conducting thorough assessments, and formulating evidence-based plans.
When documenting anxiety, nurses can utilize SOAP notes to capture key information such as the patient’s self-reported symptoms and concerns in the subjective section. For example, they may note the patient’s persistent worry, restlessness, and difficulty concentrating. In the objective section, measurable data such as increased heart rate, trembling hands, and hyperventilation can be recorded. The assessment section can include the evaluation that anxiety disorder is suspected, and collaboration with a mental health professional is recommended. Finally, in the plan section, nurses can outline interventions like providing psychoeducation on stress management techniques, referring the patient to a therapist for cognitive-behavioral therapy, and monitoring medication adherence if prescribed.
Similarly, when addressing depression, nurses can utilize SOAP notes effectively. The subjective section can capture the patient’s self-reported feelings of sadness, loss of interest in activities, and changes in appetite. In the objective section, observations such as slumped posture, slowed motor movements, and tearfulness can be documented. The assessment section may state that the patient’s symptoms meet the criteria for major depressive disorder and suggest referral to a psychiatrist for evaluation and possible medication management. The plan section can involve implementing daily mood assessments, encouraging engagement in pleasurable activities, coordinating support groups, and collaborating with the care team for potential medication adjustment.
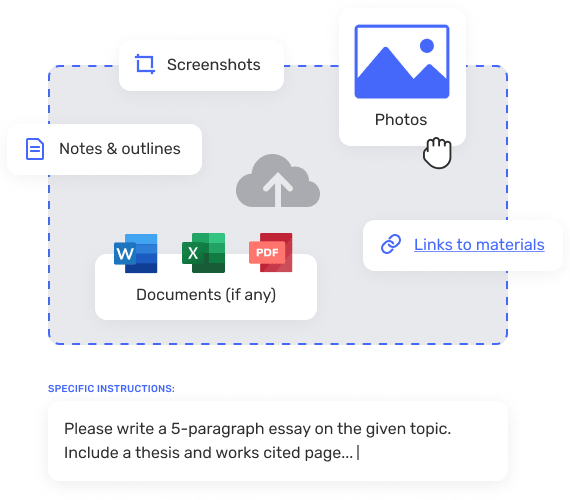
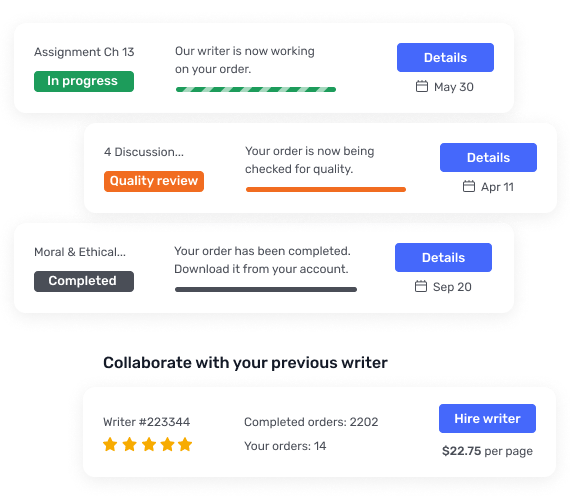
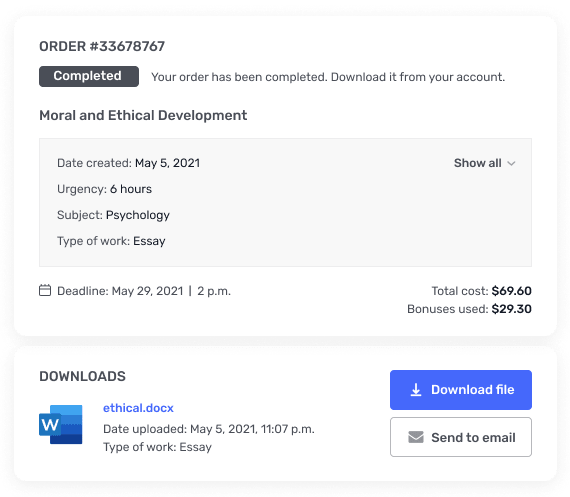
When it comes to the quality and accuracy of your nursing SOAP notes, GradeSmiths is your trusted partner. Our experienced professionals specialize in providing professional writing and editing services for nursing documentation. We understand the importance of incorporating all the necessary elements, adhering to the SOAP note format, and ensuring clarity and precision in your documentation. With GradeSmiths, you can trust that your SOAP notes will be meticulously crafted, meeting the highest standards of quality and professionalism.
Bring your anxiety and depression SOAP notes to GradeSmiths, and let our experts transform them into clear, concise, and comprehensive documents. Whether you need assistance with soap documentation, soap method charting, or creating soap notes in counseling and psychotherapy, we have the expertise to meet your needs. Contact us today and experience the difference that GradeSmiths can make in enhancing the quality of your nursing documentation and improving patient care outcomes.