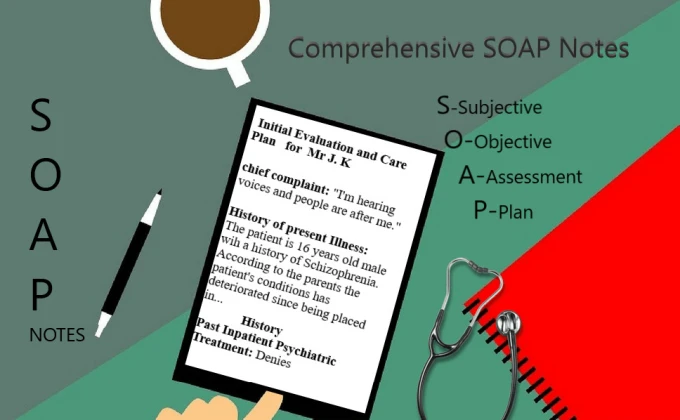
Decoding SOAP Notes: A Comprehensive Guide to Understanding SOAP Progress Notes.
Introduction
In the medical field, effective communication is crucial for the delivery of high-quality patient care. One essential aspect of communication is the documentation of patient encounters through SOAP (Subjective, Objective, Assessment, and Plan) progress notes. SOAP notes provide a standardized format for healthcare professionals to record patient information, track progress, and facilitate continuity of care. This comprehensive guide aims to demystify SOAP notes and provide a step-by-step approach to writing high-quality SOAP notes, complete with examples.
- Understanding the SOAP Note Format: SOAP notes consist of four main sections: Subjective, Objective, Assessment, and Plan. Each section serves a specific purpose and provides valuable information for both the healthcare provider and other professionals involved in the patient’s care.
a) Subjective: The Subjective section captures the patient’s account of their symptoms, concerns, and any relevant information they provide verbally. This section includes the patient’s chief complaint, medical history, and any subjective descriptions of symptoms such as pain intensity, location, or duration. It is important to document the patient’s words accurately and objectively.
Example: Subjective: Patient reports experiencing a persistent dull headache over the past week. Pain is localized to the frontal region and rates it as 5/10 on the pain scale. No associated visual changes or nausea reported.
b) Objective: The Objective section includes measurable and observable information gathered during the physical examination, diagnostic tests, and observations made by the healthcare provider. This section should be objective and free from personal interpretations.
Example: Objective: Vital signs are within normal range (BP: 120/80 mmHg, HR: 70 bpm, RR: 16 bpm, Temp: 98.6°F). Neurological examination reveals no abnormalities. No signs of tenderness or swelling on palpation of the frontal region.
c) Assessment: The Assessment section comprises the healthcare provider’s professional judgment and analysis based on the subjective and objective data collected. It includes the diagnosis or differential diagnosis, the provider’s interpretation of the patient’s condition, and any relevant findings from diagnostic tests.
Example: Assessment: Patient presents with a primary complaint of tension-type headache. No signs of migraines or other concerning neurological symptoms observed. Differential diagnosis includes stress-related headache and possible sinusitis.
d) Plan: The Plan section outlines the proposed course of action and the treatment plan for the patient. It includes medications prescribed, referrals made, diagnostic tests ordered, and any patient education or self-care instructions provided.
Example: Plan: Recommended over-the-counter pain relief medication and advised stress management techniques. Patient instructed to monitor symptoms and follow up if symptoms worsen or persist for more than two weeks.
- Tips for Writing High-Quality SOAP Notes:
a) Be Concise and Clear: Use concise and precise language to convey relevant information. Avoid unnecessary jargon or acronyms that may not be universally understood.
b) Use Objective Language: Maintain objectivity throughout the SOAP note. Clearly differentiate between the patient’s subjective information and the healthcare provider’s objective findings and assessments.
c) Provide Sufficient Detail: Include specific details about symptoms, physical examination findings, and test results. This helps ensure accurate understanding and facilitates continuity of care.
d) Use Appropriate Terminology: Use medical terminology correctly, but also consider the patient’s level of understanding. Explain complex terms when necessary to enhance patient comprehension.
e) Use a Structured Approach: Follow a consistent structure and order when documenting SOAP notes. This helps streamline the information and makes it easier for other healthcare providers to review and understand the patient’s progress.
Conclusion
SOAP notes play a vital role in effective healthcare communication and documentation. By following the guidelines outlined in this comprehensive guide, healthcare professionals can create high-quality SOAP.
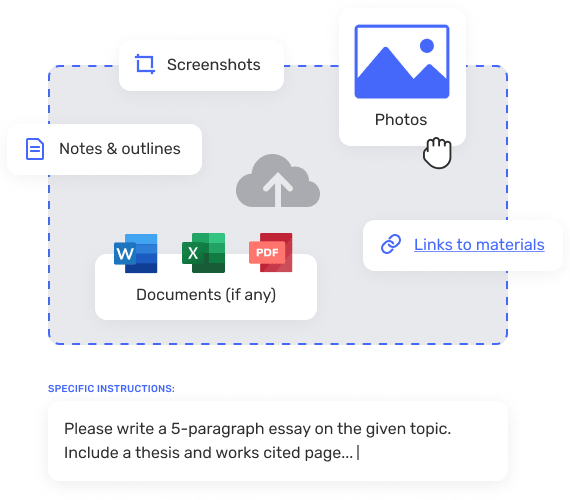
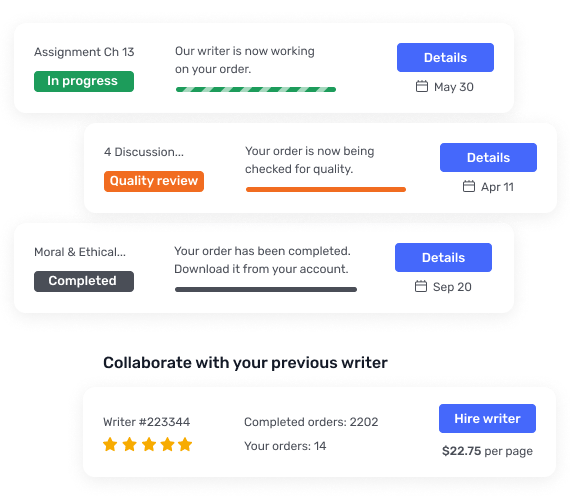
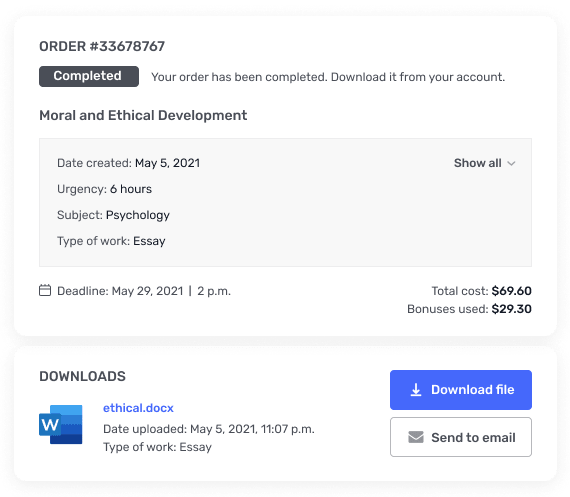
GradeSmiths, Your Ultimate Help to Writing SOAP Notes!
Do you find it a burden and a waste of time to write SOAP notes? Stop right there! GradeSmiths is ready to help with all of your paperwork hassles. Our staff of seasoned medical experts appreciates the value of thorough and precise SOAP notes. In order to save time and make sure your SOAP notes are of the best quality, bring them to GradeSmiths. Our trained experts will examine, modify, and polish your SOAP notes until they are clear, organized, and free of mistakes. By entrusting the time-consuming chore of SOAP note writing to GradeSmiths, you can devote your attention where it is most needed — to delivering exceptional patient care. Put your faith in GradeSmiths to improve the quality of your paperwork while enjoying our hassle-free services. Stop by GradeSmiths today with your SOAP notes, and we’ll take care of the rest.